What are CCDS?
Cerebral Creatine Deficiency Syndromes (CCDS) are a group of inborn errors of creatine metabolism including AGAT, CTD, and GAMT. Symptoms may include: intellectual delays, expressive speech and language delay, autistic-like behavior, hyperactivity, seizures, projectile vomiting in infancy, failure to thrive, and movement disorders.
Creatine helps supply energy to all cells in the body. It helps increase adenosine triphosphate (ATP).
Creatine is produced in the liver, which makes it out of three amino acids: arginine, glycine and methionine. Most of our body’s creatine (approximately 95%) is stored in the muscles that support the skeleton.
Normal Creatine Production Pathway:
Creatine is essential to sustain the high energy levels needed for muscle and brain development.
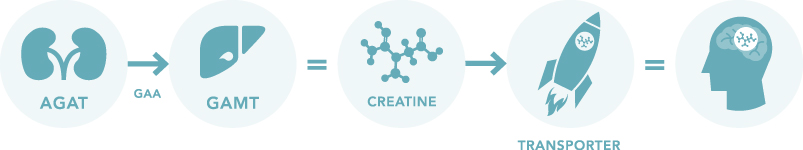
Creatine is created and delivered to the cells of the body in a three step process:
- The AGAT enzyme breaks down arginine from the diet, producing GAA.
- The GAMT enzyme utilizes GAA to form creatine.
- Creatine Transporters move creatine into the cells of the brain and muscles for use.
Creatine is necessary to increase adenosine triphosphate (ATP), providing energy to all the cells in the body.
Cerebral Creatine Deficiency Syndromes
Cerebral Creatine Deficiency Syndromes (CCDS) are inborn errors of metabolism, which interrupt the formation or transportation of creatine. There are three CCDS and their pathways are shown below.
L-Arginine:Glycine Amidinotransferase (AGAT) Deficiency

Mutations found in the GATM gene result in AGAT Deficiency.
Patients with AGAT Deficiency lack the first enzyme necessary for creating creatine.
Treatment with oral supplementation of creatine monohydrate is effective in replenishing the body’s needed creatine supply and greatly improves outcomes if initiated early for AGAT Deficiency patients. Diet restrictions are not typically recommended for AGAT patients.
AGAT patients typically have less severe symptoms in comparison to GAMT and CTD because they have functioning transporters to utilize creatine found naturally in the diet and they do not have a buildup of GAA.
Guanidinoacetate Methyltransferase (GAMT) Deficiency

Mutations in the GAMT gene cause GAMT Deficiency.
Due to a lack of the GAMT enzyme, patients with GAMT are unable to break down the GAA formed in the first step of creatine synthesis. This results in a buildup of guanidinoacetate (GAA) which is believed to be toxic to the brain at high levels.
Treatment is aimed at reducing GAA production and supplying the creatine that is not produced by the body. Patients are typically prescribed oral supplements of creatine monohydrate and l-ornithine. Some physicians also recommend diet restrictions and sodium benzoate supplementation to further minimize GAA accumulation.
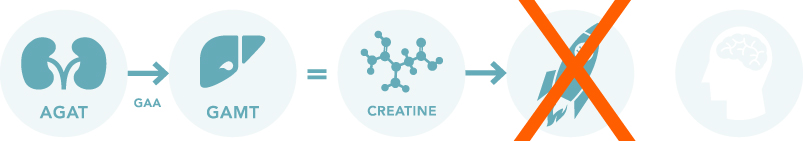
Creatine Transporter Deficiency (CTD)
CTD is also referred to as SLC6A8 Deficiency, CRTR, and X-linked Creatine Transporter Deficiency.
Mutations in the SLC6A8 gene result in CTD.
While patients with CTD have the necessary AGAT and GAMT enzymes to form creatine, the creatine transporter does not function properly. This results in creatine in the bloodstream, but not in the brain and muscles.
CTD patients do not experience high levels of GAA like GAMT patients and are not typically prescribed a restricted diet.
To date, there is no proven treatment for CTD. Visit our Research page to learn more about our intitiatives to find a cure for CTD!
Additional Information
CCDS Symptoms
The most common CCDS symptoms are listed below.
- Speech delay may be particularly severe and appears to be present in all untreated children. Some individuals develop no speech or speak only in single words.
- Global Developmental Delay affects young children with these disorders. It may be the first sign, appearing before other symptoms.
- Intellectual Disability of variable severity is typically present in all older children and adults.
- Seizure disorders have a variable age of onset and severity and are not always present.
- Hypotonia, muscle weakness, and muscle hypotrophy are common.
- Behavior disorders including autism-like behaviors and hyperactivity often occur.
- Movement disorder including dystonia and dyskinesia (sometimes labeled as cerebral palsy) may be present.
- Gastrointestinal problems such as chronic constipation and vomiting are common, especially in children with CTD.
- Failure to thrive is a term often used to describe CCDS patients.
Initial Diagnoses
It is often many years before the CCDS patient is diagnosed due to the non-specific symptoms of the disorders and the lack of clear dysmorphic features. CCDS patients are often first diagnosed with other disorders, including:
- Developmental Delay/Disability
- Failure to Thrive
- Cerebral Palsy
- Unknown Mitochondrial Disorder
- Movement Disorders
- Gastrointestinal Disorders
- Epilepsy
- Autism
View Clinician Screening recommendations.
CCDS Prevalence
The exact prevalence of Cerebral Creatine Deficiency Syndromes is unknown. Yet, sources estimate that approximately 1% of individuals with intellectual disabilities of unknown origin may have a Cerebral Creatine Deficiency Syndrome. It is also estimated that Creatine Transporter Deficiency (CTD) represents the second largest cause of x-linked mental disability behind Fragile X syndrome. There are more than 100 documented cases of GAMT Deficiency. AGAT is the rarest of the CCDS with only a few dozen known cases.
Frequently Asked Questions
-
What are the symptoms of CCDS?
Speech delay is one of the most pronounced symptoms of all three CCDS. Other symptoms can include but are not limited to: developmental delay/disability, hypotonia, movement disorders, feeding intolerances, hyperactivity, expressive speech and language delay, seizures, and autistic-like behavior. It is encouraged that an individual with any of these presentations is screened for CCDS as early as possible.
-
What should I do if I suspect my child has CCDS?
Proper diagnosis and early intervention are critical to establishing treatments needed to improve life quality and longevity for the CCDS patient. If you suspect that your child might have a CCDS, discuss symptoms and screening with your child’s doctor. Learn more on our Symptoms & Screening page.
-
How do you test for CCDS?
Initial screening for CCDS is noninvasive and is possible by measuring guanidinoacetate (GAA), creatine (Cr), and creatinine (Crn) in plasma and urine. Follow up genomic testing and brain MRI with spectroscopy may be ordered to confirm CCDS diagnosis. For more information regarding CCDS screening, consult your child’s doctor. A listing of laboratories that perform CCDS testing can be found here.
-
What specialists screen for CCDS?
Many pediatric neurologists and geneticists are able to perform initial CCDS screening. If your child is experiencing CCDS symptoms, talk to your primary care provider about consulting a child neurologist or geneticist.
-
Is CCDS ever misdiagnosed?
CCDS patients are frequently misdiagnosed with cerebral palsy as infants and toddlers. Children are often diagnosed with autism or developmental delay. If your child has been diagnosed with cerebral palsy, failure to thrive, developmental delay/disability, Autism, or Mitochondrial disorder, ask about screening for CCDS.
CCDS Medical References
NIH GeneReview | A review of the three CCDS from the NIH
Genetics Home Reference | National Library of Medicine’s overview of AGAT
Science Direct | AGAT: Clinical presentation and response to treatment in two patients with a novel mutation
Think Genetic | An Overview of GAMT
Genetics Home Reference | GAMT Information from the National Library of Medicine
Science Direct | GAMT: Outcomes in 48 individuals
Genetics Home Reference | The National Library of Medicine’s review of CTD
Orphanet | An overview of CTD by Orphanet
Journal of Pediatrics | Early Indicators of Creatine Transporter