Creatine Decoded: Behavior Support and the First ACD Webinar for Parents
This essay was written by Celeste Graham, ACD Director of Education with support from Laura Trutoiu, ACD Director of Research and Heidi Wallis, ACD President.
#CreatineDecoded is a quarterly educational essay series that sheds light on research relevant for Cerebral Creatine Deficiency Syndromes (CCDS). The essays feature community contributors, often parents, who with the help of the ACD, explore in their own words the CCDS science you want to know more about. Have a topic in mind? Send suggestions to Laura Trutoiu, ACD Director of Research auract@creatineinfo.org.
Education is one of the key parts of our mission here at the ACD. This “Creatine Decoded” blog post gives a brief overview of a topic near and dear to many of us as CCDS parents: what science and psychological theory say about what therapies work for our kiddos related to their behaviors. The ACD recently held a webinar focused on supporting parents in the CCDS community in regards to challenging behaviors. I’m not sure about you, but we have seen an increase in behaviors the past few months in our house!
Judi Miller (Children’s Hospital of Pennsylvania) and Audrey Thurm (National Institutes of Health) were hosts of the webinar and offered valuable reminders and insightful strategies in managing difficult behaviors that many in our CCDS community struggle with. Both Judi and Audrey have a wealth of experience in working with children with Intellectual Disability, Autism, and children who have Cerebral Creatine Deficiency Syndromes. They both are also part of the Vigilan CTD Study: Judi is the Principal Investigator for the overall study, and Audrey is a key investigator at the NIH.
First, let’s do a quick summary of what is known about behavior support from a scientific perspective. A common approach to working through behaviors is Applied Behavioral Analysis therapy (ABA), and behavioral therapy more broadly. ABA is a therapy approach that focuses on the science of learning and behavior–and working through behaviors in real-life situations: increasing desired behaviors, decreasing undesired behaviors, and working on skills. In ABA, often a Board-Certified Behavioral Analyst (BCBA)may do an assessment with your child and then develop a plan containing goals for a therapist to work on with your child. Parents are typically involved in plan development, as it is a team approach. Unfortunately, ABA is expensive and often only covered by insurance with a specific diagnosis (i.e. Autism Spectrum Disorder). There is usually a long waitlist to begin services and it involves a significant time commitment; it is also a bit intrusive, as it involves therapists coming into your home 4-5 days/week for 3-4 hours. ABA has also received some criticism, primarily because older methods of the therapy were a more rigid approach to learning. There are many studies on the effectiveness of ABA in education and the first article that showed the benefits for children with autism spectrum disorders dates back to 1987 (Lovaas).
ABA is not the only form of behavioral support, and though it has a lot of science behind it, there are other approaches out there. For example, Verbal Behavior Therapy is a therapy approach that teaches communication and language, helping to connect why we use words and how they are useful–connecting words with their purpose. Similarly, some people choose to see a behavioral therapist (a therapy approach that involves meeting with a trained therapist to identify and work through behaviors through various methods, depending on how the therapist is trained) to name a few.
Next, let’s get to the webinar! After brief introductions and a few surveys to gauge the audience, the interactive webinar began. Just a quick side note…it was so great to see and interact with everyone on the screen! ☺
Here are some take-aways from the presentation and discussion:
- Disclaimer:
- EVERYONE is melting down right now…most kids were done in May 2020 and adults are done now—especially with the rules about wearing masks. There are no judgments in how we are handling behaviors—we’re all doing the best we can!
- Managing Expectations:
- Managing Tantrums:
- Look at your child’s daily rhythm and the big picture of their day—could they be hungry/angry/lonely/tired (easily remembered by the acronym H.A.L.T.)?
- Strategy for working through a tantrum (if safety, not a concern) = planned ignoring of the tantrum, NOT child—this looks like giving them no interaction (while keeping them safe)…then, you start doing something nearby and when they come over, welcome them into the activity with no fanfare.
- Negative Attention Seeking:
- Some kids can’t tell the difference between positive and negative attention, so they seek attention however they can get it.
- Most kids would rather have negative attention than no attention.
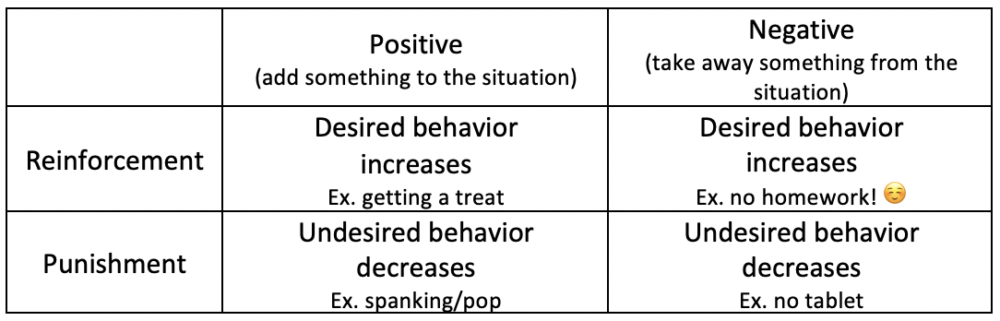
- Reinforcement and Punishment:
- The goal is to increase desired behaviors while decreasing undesired behaviors.
- Severe Attention Seeking Behavior:
- Even though planned ignoring is a great way to reduce attention-seeking behaviors, sometimes it’s not possible to get EVERYONE to ignore the behaviors. Siblings, frustrated family members, neighbors, or people in the community might give your child attention to negative behaviors. Train the folks you can and celebrate with them when they make an effort!
- Q&A:
- If possible, it is beneficial to work with a team of therapists to collaboratively work through specific aspects of behaviors and communication barriers…ABA/behavioral therapist, speech therapist, occupational therapist, physical therapist.
- Potential topics for additional webinars in the future = puberty and behaviors, improving communication.
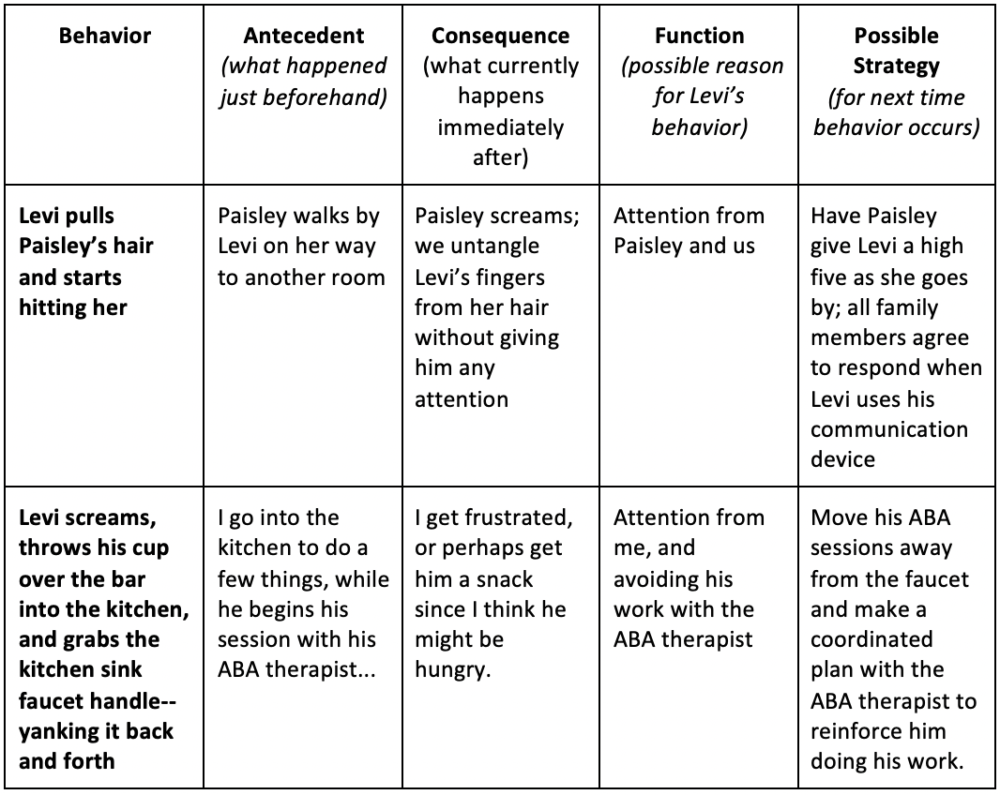
- There was some discussion of a Functional Behavioral Assessment (FBA)…this is where someone comes in and observes behavior (antecedent-what happens before the behavior/behavior/consequence-what happens after the behavior), trying to assess the function behind the undesired behaviors. This should be someone trained in FBA’s.
As always, time ran out quickly! However, I think there were plenty of things to think about as we examine our child’s challenging behaviors—and our reactions to them. It is always great to gather as a CCDS community…and it is amazing to be able to have conversations with clinicians who are familiar with our CCDS kids. We’d love to hear from you if we should pursue making this a regularly recurring series! :)
Lastly, as a special education teacher, here are a few tidbits I’d like to reiterate…
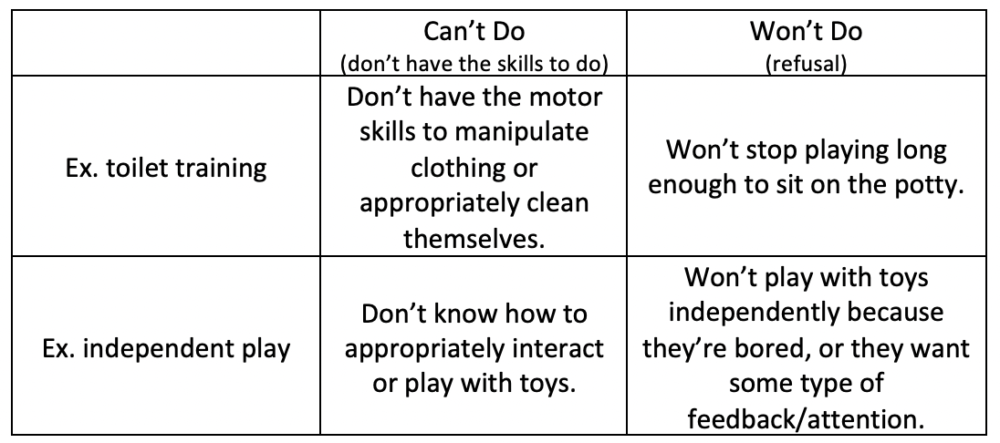
- Finding the function of behavior is important in figuring out how to work through it…
- Here are a few examples:
- Visual supports go a long way! I have noticed that for kids I work with, as well as Levi, it helps if they SEE it…
- visual schedule–so they can see what comes next (i.e. diaper, eat, Blippi or work, snack, work, outside…or even as simple as “first”/”then”)
- token board–so they can see what they are working for (have them choose from a few options that are available) and how many more things they have to do in order to earn their reward
- red/green circles–we use this to show what is available and not available (i.e. posted on doors throughout the house with velcro; I’ve also used this with choices he’s picked for a snack)
- visual timer–so they can see how long they have of a reward before a transition; I’ve also used counting down from 10 with my fingers to help Levi calm down during a tantrum
- Varying your prompting levels can sometimes help diffuse a situation.
- For example, I have noticed that when I take Levi to his room to change his diaper and put him to bed, he thrives (and giggles) if I try to lift him or use a certain tone of voice. I have started trying to take the physical and verbal prompting out of the situation, replacing it with gestural prompts (i.e. snapping to get his attention and pointing to where I want him to be)–not giving him direct eye contact. It may take him a few minutes, but he *typically* will come and lay down.
- Prompting levels:
- physical = hand over hand, physically supporting them to do the task you need them to do
- partial physical = still physically touching/guiding them, but not completely
- model = you model a task (what you want them to do)
- verbal = orally stating what you want them to do
- partial verbal = still orally stating things, but it might just be one or two words or a sound
- visual = using some type of visual to show them they need to do a task or what they are working for
- gestural = pointing, waving, or doing some type of action to get them to do a task
- partial gestural = not as obvious could even be an eye gaze
- Tantrums…where do I start! The main goal is to keep you and your child safe while decreasing the behavior.
- For example, Levi’s tantrums often include hitting his head/headbanging, screaming, hitting, and pulling hair. When he starts in to his tantrum, I get to him as quickly as possible, without offering any type of attention (i.e. verbally). I block his head from hitting anything–with my hand or a pillow. I also block him from hitting me, running into me, or throwing objects by diverting him. I am usually anticipating what he is going to do. Sometimes, I give him some deep pressure–which tells me that he needs more sensory input (which he tends to need a HIGH level to input frequently). Other times, I calmly tell him to use his words, start counting down from 10, or redirect his attention. Occasionally, I will put his helmet on him to keep his head safe, which distracts him just enough because he is ticklish under his neck.
Hang in there, ACD family! We’re in this together…while we may be spread apart, it definitely helps to know that there are others who are going through the same struggles! I CAN’T WAIT to see you in person at the Symposium in Utah next June!! Feel free to email me at celeste@creatineinfo.org with any questions… I’ll do my best to help!!! (Just a disclaimer that I am a parent and special education teacher in NC. This blog post was written from these perspectives so be sure to discuss any suggestions with your care team!)
References:
Lovaas, O. I. (1987). Behavioral treatment and normal educational and intellectual functioning in young autistic children. Journal of consulting and clinical psychology, 55(1), 3.